Transplantation of pancreatic islet cells could revolutionize the treatment of diabetes mellitus, if transplant survival could be improved. Inflammation, immune rejection, and recurrence of autoimmunity can contribute to loss of transplanted cells. Leukocytes activated by such an immune response have been shown to attack and damage the local microvasculature, leading to perfusion failure. Unfortunately, current clinical tools to monitor graft health often identify problems too late for intervention. Earlier, noninvasive detection methods are needed to improve outcomes.
Immune rejection after pancreatic islet cell transplantation: in vivo dual contrast-enhanced MR imaging in a mouse model.
Wang et al. present a magnetic resonance imaging (MRI) method to monitor vascular changes following islet cell transplantation in vivo. The researchers use a long-circulating T1 contrast agent that accumulates at sites of inflammation featuring disruption of capillary integrity. The imaging agent consists of a protected graft co-polymer (PGC) covalently linked to gadolinium– diethylenetriaminepentaacetic acid with fluorescein isothiocyanate (PGC-Gd-DTPA-F).
To demonstrate the passive accumulation of the contrast agent at sites of immune-mediated vascular disruption, the researchers co-localized fluorescin-labeled PGC-Gd-DTPA-F and islet cells labeled with superparamagnetic dextran-coated iron oxide nanoparticles by MRI. The team performed in vivo imaging of diabetic mice transplanted with the islet cells, one day before and seven days after rejection was induced. Using a 9.4 T Bruker BioSpec horizontal bore MRI system with a custom coil and ParaVision 5.1 Software, the researchers acquired gradient echo T2-weighted sequence images followed by precontrast and PGC-Gd-DTPA-F–enhanced T1-weighted images.
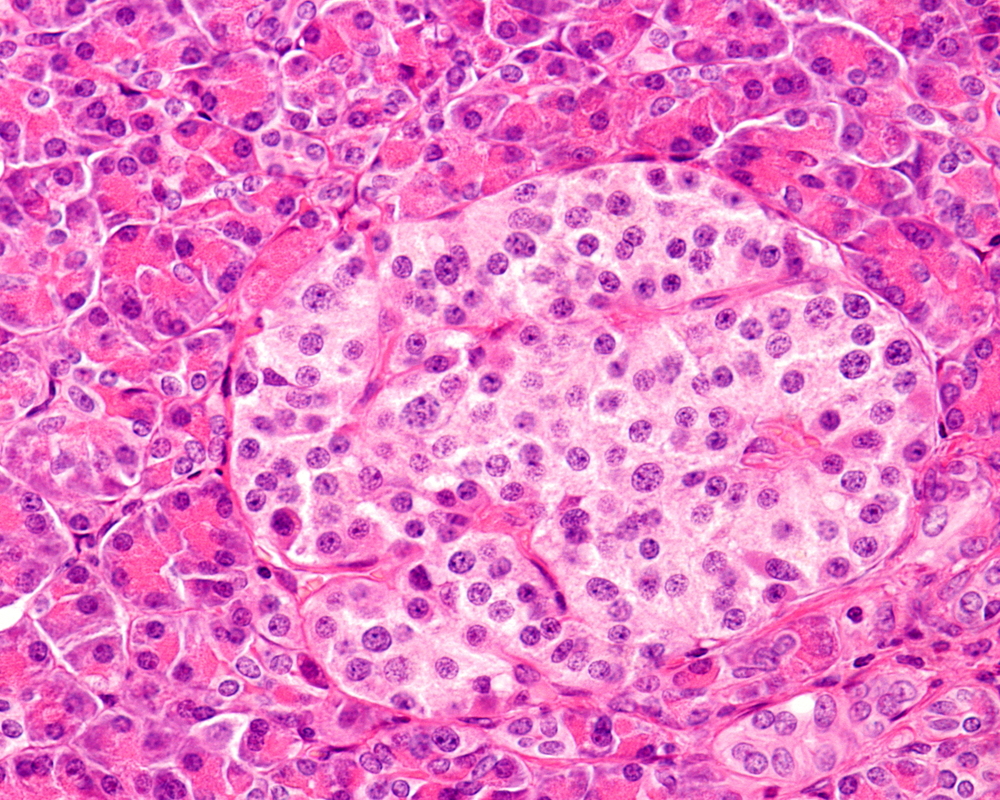
PGC-Gd-DTPA-F appeared as a high-intensity signal in the graft area of animals undergoing rejection, as shown in the T1-weighted images. That signal co-localized with a low-intensity area in the T2-weighted images, showing the iron-oxide labeled islet cells. The PGC-Gd-DTPA-F signal was absent in animals not induced to reject the grafts. The authors confirmed by histology that the T1-weighted signal reflects PGC-Gd-DTPA-F accumulation at sites of vascular deterioration resulting from immune rejection of the transplanted islet cells.
The author’s dual-contrast approach using the Bruker BioSpec MRI system successfully co-localized transplanted islet cells with a site of immune rejection in diabetic mice, providing proof-of-concept for a potentially valuable clinical monitoring tool.
Reference
Wang P, Schuetz C, Ross A, Dai G, Markmann JF, Moore A.
Radiology. 2013 Mar;266(3):822-30. Epub 2012 Dec 21. PubMed Central: PMC3579171.