A Promising Approach to a Deadly Disease
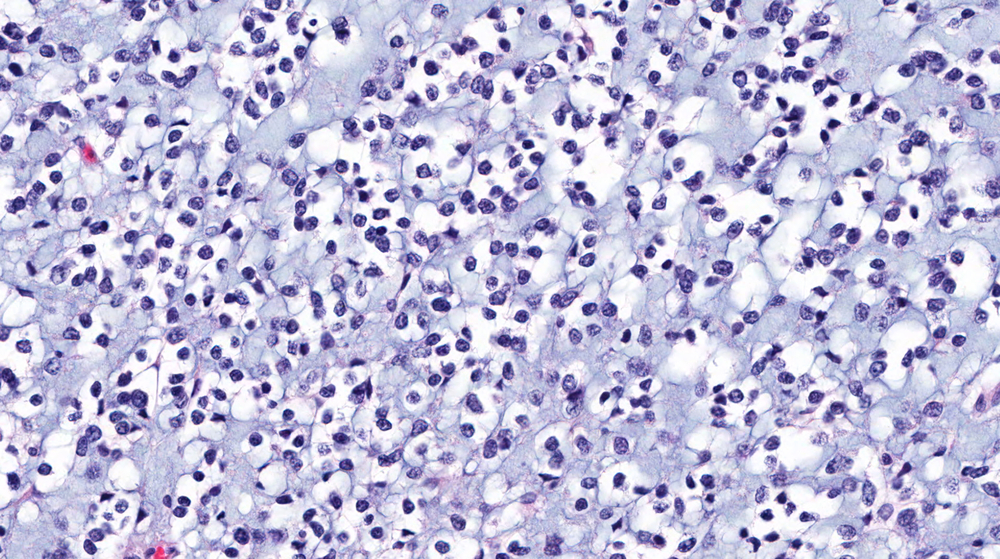
The most common type of central nervous system tumor, glioblastoma multiforme is an aggressive cancer with mean survival of only 15 months from diagnosis; its localization to the brain and tendency to spread quickly limit treatment options and effectiveness. Standard therapy includes surgery followed by radio- and chemotherapy. Unfortunately, even with this combination, long-term tumor control is possible in as few as one-in-five patients.
Tumor growth depends heavily on creation of new blood vessels. Anti-angiogenic drugs have shown promise in preclinical studies as agents to sensitize tumors to chemo- and radiotherapy. Perhaps supplementation with such a drug could improve the outlook for glioblastoma patients.
Recent studies have associated astrocytomas such as glioblastoma with elevated expression of vascular endothelial growth factor (VEGF), which encourages angiogenesis, as well as progesterone receptors, which mediate an increase in both VEGF expression and tumor growth. The anti-progestin and anti-glucocorticoid drug mifepristone shows anti-tumor activity in breast and ovarian cancers, and has also been associated with decreased VEGF expression in prostate cancer cells. Could mifepristone improve outcomes in glioblastoma?
Llaguno-Munive and colleagues tested the effects of mifepristone on tumor growth and VEGF expression in vivo. Mice with glioblastoma xenografts were treated with radiation therapy, with or without temozolamide chemotherapy and/or mifepristone. Control mice received no treatment. Measuring tumor size weekly using calipers, the authors found significant reductions in tumor growth after 15–20 days of treatment supplemented by mifepristone, relative to non-mifepristone treatment groups and controls.
The researchers tracked metabolic tumor volume as reflected in 18F-fludeoxyglucose (FDG) uptake by tumor cells, using microPET and X-ray computed tomography (CT) imaging on a Bruker Albira multimodal imaging system. FDG uptake was measured using the volume of interest – the volume concentration of the radio-labeled FDG – across the entire tumor volume, using PMOD software (PMOD Technologies, Ltd.). The mifepristone treatment groups showed a trend toward smaller metabolic tumor volumes, with a statistically significant improvement versus radiation therapy alone. All treatments were associated with reduced VEGF expression versus controls, measured by polymerase chain reaction.
Mifepristone showed promising activity as a chemo-radiotherapy sensitizing agent in this in vivo study, without signs of systemic toxicity. Simultaneous administration of mifepristone with radiation therapy and temozolamide chemotherapy produced a significantly greater anti-tumor effect compared to radiation or combined radiation and chemotherapy alone. The authors conclude that mifepristone is a good candidate to improve the effectiveness of chemo-radiotherapy in glioblastoma, a new hope for patients in great need.
Reference
Monserrat Llaguno-Munive, Luis Alberto Medina, Rafael Jurado, Mario Romero-Piña, and Patricia Garcia-Lopez. Mifepristone improves chemo-radiation response in glioblastoma xenografts. Cancer Cell Int. 2013; 13: 29. PMCID: PMC3626552.